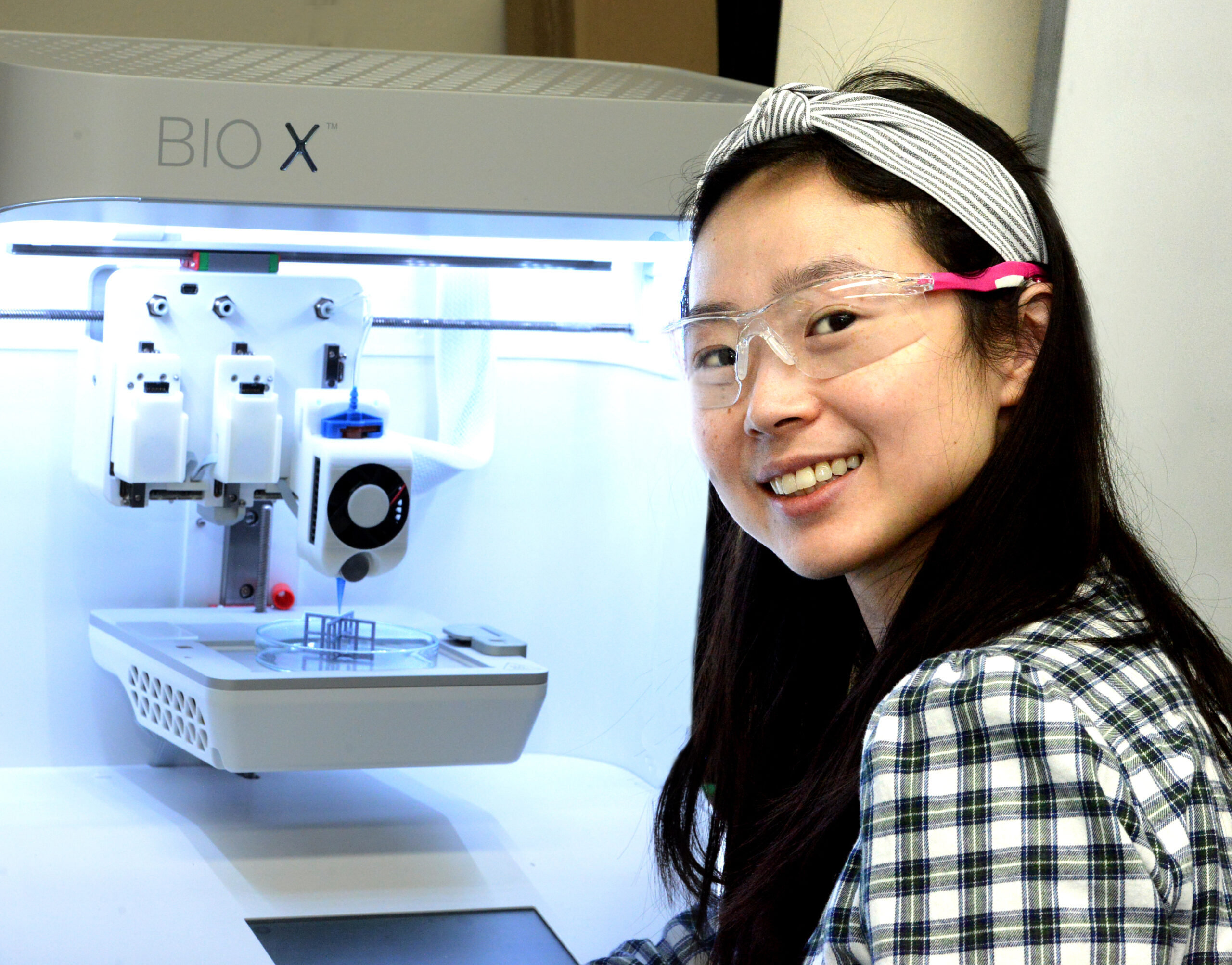
Grace Gu
Mechanical EngineeringGrace Gu is an Assistant Professor of Mechanical Engineering at UC Berkeley. She earned her BS in Mechanical Engineering from the University of Michigan and her MS and PhD from the Massachusetts Institute of Technology.
Spark Award Project
Her research interests include composites, additive manufacturing, fracture mechanics, topology optimization, machine learning, finite element analysis, and bioinspired materials. For her Bakar Project, she is focusing on 3D printing materials that can be integrated with medical technology.
Grace Gu’s Story
Racing downslope, she makes a quick turn. Her skis skid on the snow, and she feels a “pop” in her knee as it gives way. That’s the telltale sound of a tear in the knee’s anterior cruciate ligament – the ACL. Her skiing is over for the season, maybe longer.
The ACL is an inch-long bundle of collagen fibers that connects thighbone to shinbone, stabilizing the knee. Suddenly stopping or twisting the knee on the ski slope or soccer field can stress the ligament to the tearing point.
More than 100,000 people a year in the U.S. rupture their ACL. Most are sports injuries but the ligament can potentially tear from any sudden twist of the knee.
If rest, ice and then physical therapy don’t do the job, surgery is the next option to reconnect the ligament to the ends of the two bones.
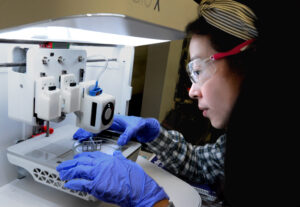
Grace Gu, assistant professor of mechanical engineering, thinks there’s a better way. She aims to make a replacement part – precisely fabricating a new ligament from collagen or other materials using 3D “bioprinting.” Her technology will enable automatic adjustments of the printing process in real time using AI to both perfect the ligament’s 3D shape and modify its structure.
She describes her Bakar Fellows Program research project aimed at delivering a prototype 3D-printed ligament in three years.
Q) For starters, how does 3D bioprinting work?
A) 3D printing is actually a series of 2D printing. We print layer by layer to build up the 3D object or structure. We are using what is called direct ink writing, where inks are deposited under controlled flow rates or pressure.
You first need a blueprint – a digital file created with a modelling software. The computer-generated model is sent to the printer to become a physical model.
What is the equivalent of ink in your 3D ligament printing?
We intend to use collagen-based materials to print most of the synthetic ligament prototype. Collagen is available as an ink, in the form of a material that can swell with water to make a kind of Jell-O called a hydrogel. The collagen material is extruded through a nozzle – like squeezing toothpaste from a tube under pressure.
What are the limitations of current ACL replacement surgery that you hope to overcome with 3D bioprinting?
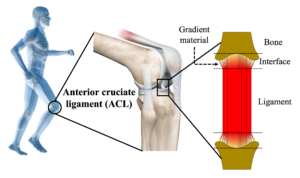
The major concern is that while fractures of bone usually mend fairly quickly, ligament-to-bone injuries heal much more slowly. Bone is much stiffer than ligament—about 100-1000 times stiffer. If you take two really different materials and bring them together, it’s not going to transfer the load very well.
Our 3D bioprinting technology will enable us produce what we call a gradient interface in which the final sliver of ligament at each end – a tiny fraction of its total length – becomes increasingly stiffer, more like bone. That will provide good adherence and promote more durable healing.
How will you accomplish this?
With our Bakar Fellows Program Spark Award, we will be using a combination of three methods to create the gradient interface. The first is by mixing different concentrations of materials. The second is to use the same material but modify its structural design such as introducing porosity. Lastly, we can change the parameters of the printing process such as nozzle temperature, printing speed, and pressure. We have found that these parameters can have a large effect on the properties of printed materials.
How do you direct the printing process to make the ligament with the desired size, shape and properties?
We have developed optimization algorithms that will help guide us on emulating the shape and resilience of native ACLs. The printing technology will include cameras and sensors to track the progress of the printing in real time and direct it to automatically self-correct if the structure that it is building up is not matching our blueprint.
I know collagen is largely protein – not a lot of cells. But bone tissue is made of living cells. How does the new bone-like material at the tips of the new ligament become living bone, like the native bone?
The best case scenario would be if the body’s own bone cells migrate, or repopulate the new scaffold. If that isn’t successful, we will be looking into seeding our 3D-printed bone component with healthy bone cells from the patient’s body.
If you are successful, how do you see your 3D bioprinting fitting into the surgical setting?
The dream would be a company with branches near hospitals. The surgeons could take a scan of the patient’s torn ligament and send it to us, and we will design and fabricate on demand and send it back to the hospital within hours. The fabricated synthetic ligament would be tailored and optimized for each patient. This is the future we envision that our technology will integrate with medicine.