
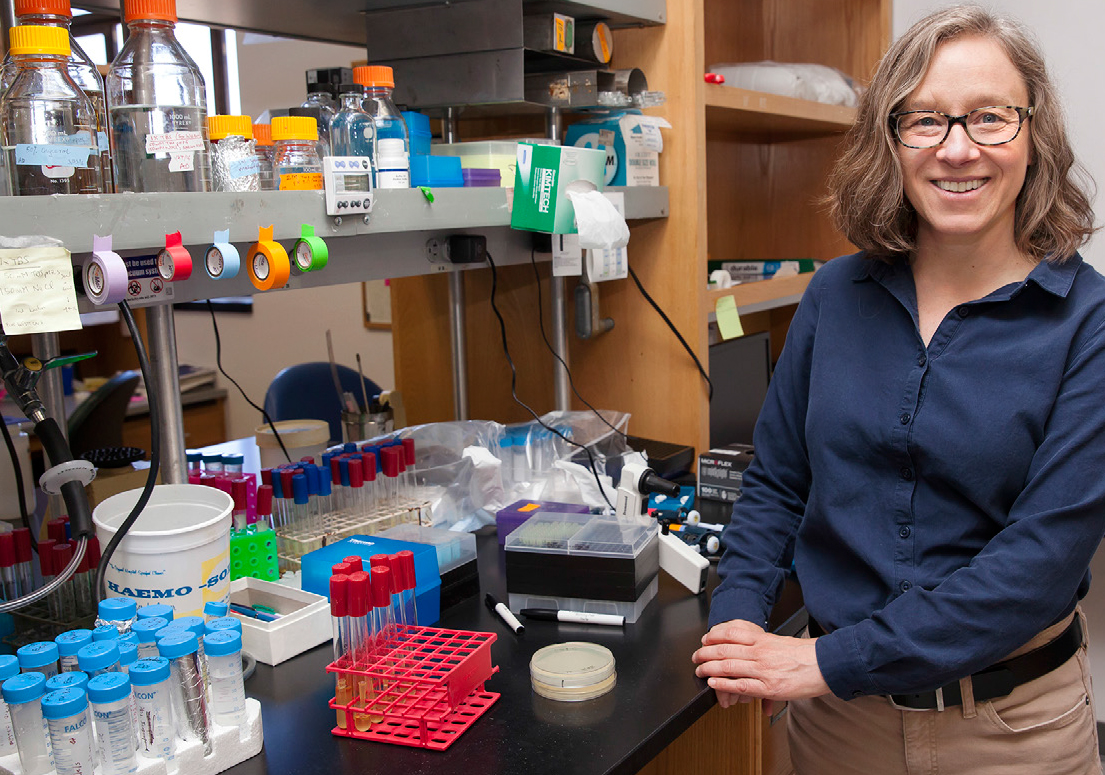
Kathy Collins
Molecular and Cell BiologyKathleen Collins is a Professor in the Department of Molecular and Cell Biology.
Project Description
New Reverse Transcriptase Technologies: Tools for Diagnosis and Health Status
Molecular signatures of an individual’s current heath status remain largely unread, at enormous cost. DNA sequence tests can inform disease risk but rarely report on current health. RNA sequence has the promise to meet the need for a broadly informative, readily interpretable, and affordable read-out of health status. RNA is DNA in action: quantitative and qualitative variations in RNA provide extra layers of information and are filtered for irrelevant genomic DNA sequence. Because cells secrete packets of RNA into the bloodstream, particularly cancer and dying cells, a simple blood draw will allow disease detection independent of the tumor type or type of tissue dysfunction. Our startup, KarnaTeq, has developed new tools for RNA sequencing that can be used by scientists now and health providers in the future.
Kathy Collins’ Story
The ideal non-surgical approach might start with a simple blood draw. Snippets of DNA or RNA detected in the blood could be analyzed for the presence of a tumor; whether it has metastasized and whether it carries mutations for resistance to specific drugs. Such “liquid biopsies” may now be within reach.
Kathy Collins, professor of biophysics, biochemistry, and structural biology is launching a startup called KarnaTeq to develop and market a technology to increase the diagnostic power of this new strategy.
Cancer cells commonly shed bits of DNA into the blood. In several recent cancer clinical trials, researchers isolated DNA from patients’ blood and amplified it for analysis. In a DNA study from one specialized type of treatment, they were able to identify most of the treatment-resistant mutations that had been detected through conventional, invasive biopsies. In fact, DNA sequencing revealed some mutations that the original biopsies had missed, the scientists reported.
But even a diagnostic tool as promising as this should be more sensitive and informative in order to fulfill the goal of personalized medicine, says Collins. With support from the Bakar Fellows Program, she is developing new techniques to scrutinize the total content of RNA in blood — a strategy that she thinks may add vital clues missed by DNA analysis.
“RNA is DNA in action,” Collins says. While DNA holds the blueprint for making all the proteins in the body, it hands off to RNA only the instructions that the cell needs. As a result, this “messenger RNA” carries the up-to-date information on cells’ conditions and needs.
“Sequencing RNA from liquid biopsies will allow us to see not only the state of a cancer but also the molecular signatures of any normal tissue that is in trauma from a treatment,” she says. “Tissue stress is critical to tuning therapy. DNA alone won’t yield this information.”
In other words, DNA sequences may be easier to find, she says, but they don’t hold all the clues. “We don’t want to bias our understanding by getting only a partial picture.”
To analyze gene sequences retrieved from blood, researchers use a relatively large blood draw. They isolate and amplify the genetic material that has made its way into the blood. With current technology, they can generate millions of individual DNA molecules for analysis, but not all of the RNA.
So far, Collins says, only messenger RNA from intact cells can be analyzed comprehensively. “A profile of other types of RNA such as non-coding RNA and RNA from pathogens would give an unbiased, ‘wide-field’ snapshot of current health status.”
Collins has developed a new technology that employs a type of enzyme that she has studied for more than 20 years. It is called a reverse transcriptase because it can translate, or transcribe, RNA into DNA — the reverse of the classic “Watson and Crick” DNA to RNA process.
 HIV and other retroviruses use their own reverse transcriptase to transcribe their RNA into DNA and then integrate it into a host’s DNA strands. The invaded cell then becomes an agent of its own destruction, blindly replicating the virus’s genetic instructions along with its own, enabling the virus to multiply and spread.
HIV and other retroviruses use their own reverse transcriptase to transcribe their RNA into DNA and then integrate it into a host’s DNA strands. The invaded cell then becomes an agent of its own destruction, blindly replicating the virus’s genetic instructions along with its own, enabling the virus to multiply and spread.
Through modifications of an ancient reverse transcriptase, Collins can retrieve a comprehensive inventory of RNA. Because of the unique way the enzyme engages RNA molecules, it can access folded strands generally invisible to other techniques. The transcribing process captures more of the RNA than other methods and is less error-prone.
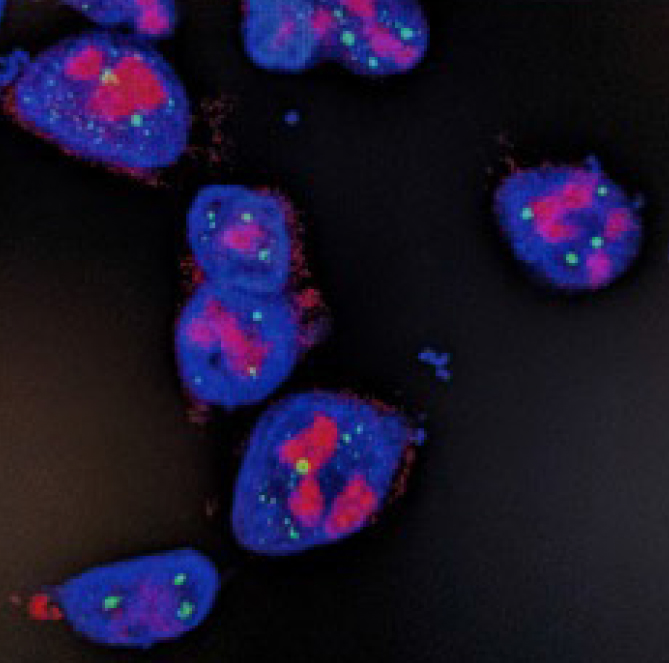
She is particularly interested in applying the new strategy to study RNA held in bubble-like vesicles, called exosomes, secreted by cancer cells into the blood. Very little is known about them, but many scientists suspect that DNA, RNA and other molecules packed inside the vesicles can provide unique insights into cancer’s progress in a patient.
With guidance from Bakar Fellows mentors, Collins aims to advance research on exosomes and other potential troves of genetic information, and expects her new RNA analysis technology will be useful in a range of basic research and clinical applications.